Email : admin@mskdoc.co.nz | Phone : 02727 00100
Opening Hours : Mon-Friday : 10 AM – 4 PM
Email : admin@mskdoc.co.nz | Phone : 02727 00100
Opening Hours : Mon-Friday : 10 AM – 4 PM
Email : admin@mskdoc.co.nz | Phone : 02727 00100 | Opening Hours : Mon-Friday : 10 AM – 4 PM
By: Dr Zaid Matti
Musculoskeletal Medicine Specialist
Osteoarthritis (OA) is a leading cause of disability worldwide, often affecting the knees, hips, and small joints. While lifestyle modifications and physical therapy are foundational treatments, injectable therapies provide targeted relief for patients with persistent symptoms who wish to delay or avoid joint replacement.
For many years, hyaluronic acid (HA) injections—also known as viscosupplementation—have been used to relieve OA symptoms. However, with the rise of platelet-rich plasma (PRP) and other biologic therapies, the role of HA has come under scrutiny. Does HA still have a place in modern OA management? The answer, supported by research, is yes—but with important qualifications.
What Is Hyaluronic Acid and How Does It Work?
Hyaluronic acid is a naturally occurring glycosaminoglycan in synovial fluid, responsible for lubrication, shock absorption, and cartilage protection. In OA, the concentration and quality of HA degrade, resulting in increased joint friction and inflammation.
Intra-articular HA injections aim to restore synovial fluid properties, improve joint biomechanics, and reduce pain.
Evidence for HA Efficacy in OA
Several meta-analyses have evaluated HA’s role, particularly in knee OA:
However, the effect sizes are generally small, and guidelines vary. While the American College of Rheumatologyremains neutral, the AAOS (2013) does not currently recommend routine use, largely due to heterogeneity in study quality.
Hyaluronic Acid in New Zealand
In New Zealand, two HA products are commonly used:
These products are not publicly funded, and patients typically pay out-of-pocket unless private insurance covers it (which is rare). This financial aspect can influence treatment decisions in clinical practice.
When Is HA a Preferred Option?
Despite the emergence of PRP, HA retains an important role, particularly in the following scenarios:
How Does PRP Compare?
PRP, unlike HA, modulates the joint’s biology. It contains growth factors such as TGF-β, PDGF, VEGF, and IGF-1that promote chondrocyte activity, reduce inflammation, and enhance joint homeostasis.
Recent evidence favours PRP over HA in efficacy:
Synergistic Use: PRP + HA Combination Therapy
The idea of combining HA’s mechanical benefits with PRP’s biologic activity has gained traction:
Clinical Summary
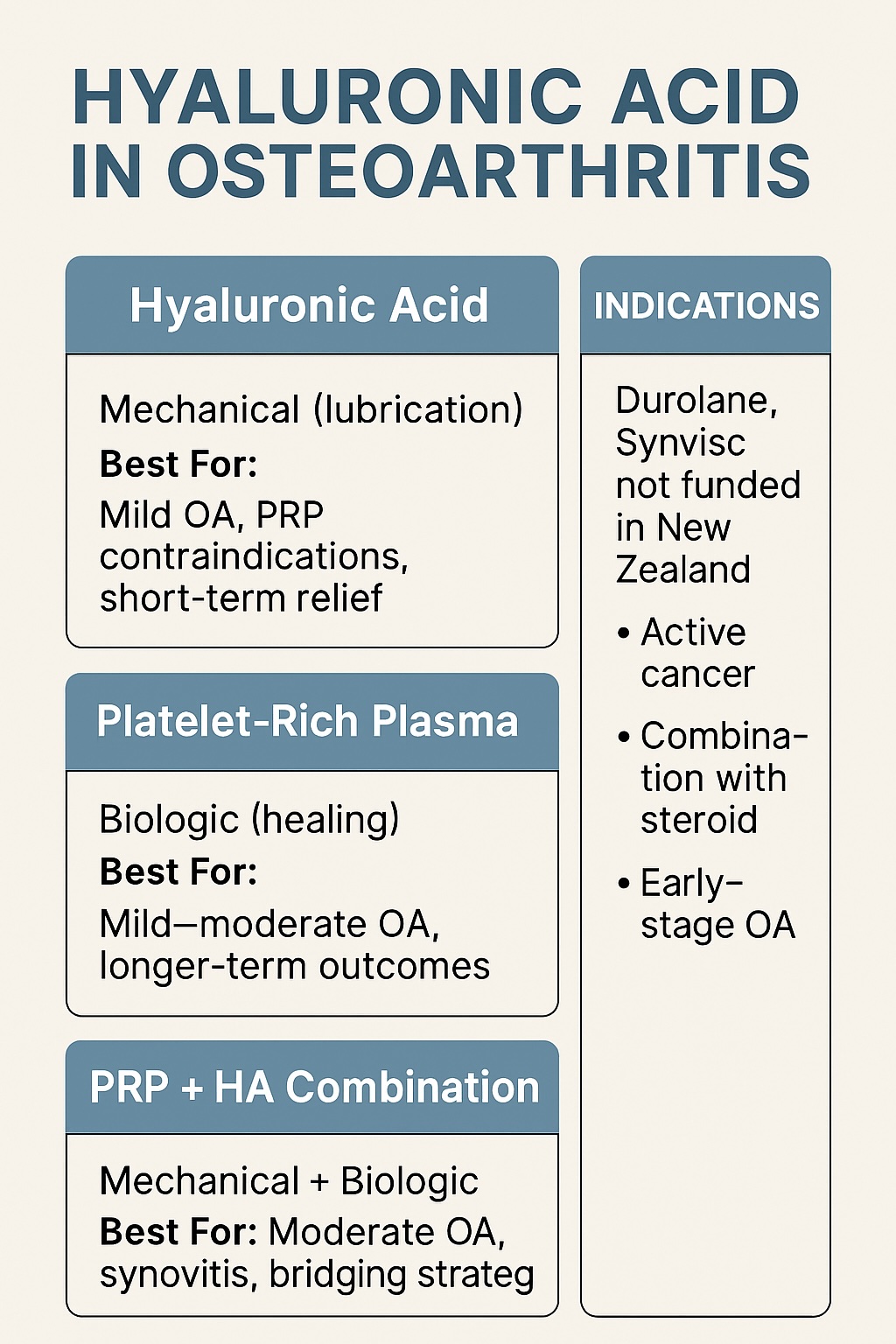
Therapy Type | Mechanism | Best For |
Hyaluronic Acid | Mechanical (lubrication) | Mild OA, PRP contraindications, short-term relief |
Platelet-Rich Plasma | Biologic (healing) | Mild–moderate OA, longer-term outcomes |
PRP + HA Combo | Mechanical + Biologic | Moderate OA, synovitis, bridging strategies |
Conclusion
While PRP is now considered the superior injectable for many OA patients, hyaluronic acid remains clinically relevant. Whether used as a safer alternative when PRP is contraindicated, or as part of a combination strategy, HA can contribute to personalised OA care. Clinicians should weigh patient goals, disease stage, comorbidities, and access when selecting therapy.
References