Email : admin@mskdoc.co.nz | Phone : 02727 00100
Opening Hours : Mon-Friday : 10 AM – 4 PM
Email : admin@mskdoc.co.nz | Phone : 02727 00100
Opening Hours : Mon-Friday : 10 AM – 4 PM
Email : admin@mskdoc.co.nz | Phone : 02727 00100 | Opening Hours : Mon-Friday : 10 AM – 4 PM
By: Dr Zaid Matti
Musculoskeletal Medicine Specialist
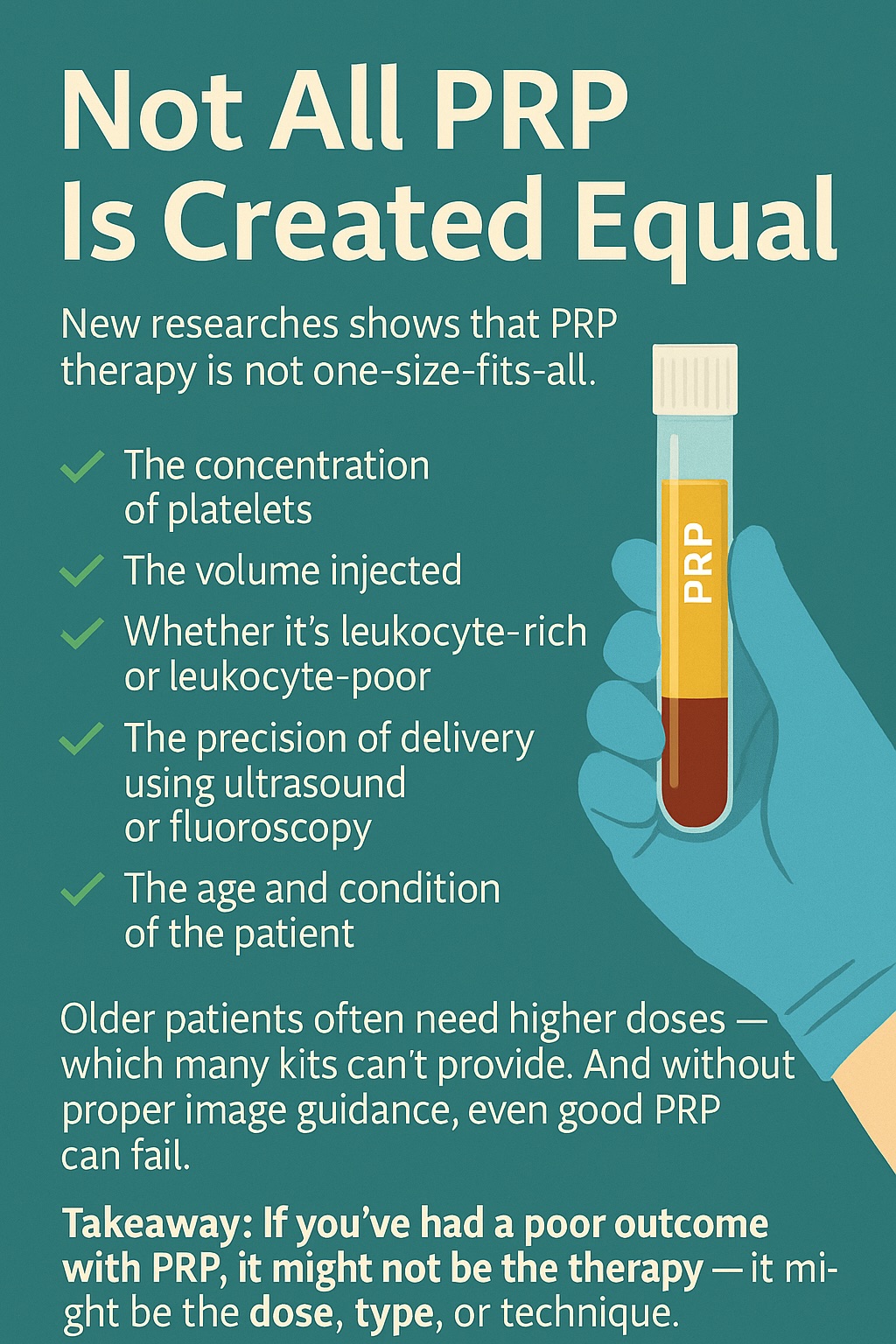
Platelet-Rich Plasma (PRP) therapy has gained widespread attention for its regenerative potential in musculoskeletal medicine — from tendon injuries to osteoarthritis and beyond. But one crucial truth often gets lost in translation:
Not all PRP is created equal.
Despite being grouped under the same name, PRP treatments can vary dramatically in their biological composition, dose, and method of administration. These differences can directly influence treatment outcomes — sometimes explaining why one patient improves significantly while another sees little or no benefit.
In recent years, our understanding of PRP has shifted significantly. Earlier studies and protocols often focused on delivering a generic platelet concentration, assuming that a basic “boost” of growth factors was enough to trigger healing.
However, more recent literature shows that therapeutic efficacy depends heavily on platelet concentration and volume:
Higher concentrations (e.g., >1 billion platelets/mL) are now correlated with improved outcomes, particularly for degenerative conditions in older adults.
Lower concentrations may be adequate for acute injuries in younger individuals with higher regenerative capacity.
Different clinical scenarios (e.g., tendon injury vs. cartilage degeneration vs. neural repair) may require customised PRP formulations in terms of leukocyte content, activation method, and dosing frequency.
In other words, blanket use of “standard PRP” is outdated and may underdeliver in many clinical settings.
Commercial PRP systems differ widely in how they concentrate platelets — and many are unable to achieve the platelet counts required for therapeutic benefit. Some systems produce PRP with only a 1.5-2× baseline concentration, which may fall short for more demanding applications like advanced osteoarthritis or chronic tendinopathies.
Furthermore, the total delivered dose (i.e., platelets per millilitre × injection volume) is often overlooked but is critical to efficacy. A low-volume injection with sub-therapeutic platelet content may simply not be enough to initiate a healing cascade — especially in tissues with limited blood supply or in aging patients with diminished regenerative capacity.
Even when optimal PRP is prepared, the method of delivery is just as important. Poorly placed PRP can render even a well-prepared product ineffective.
Key technical considerations include:
Ultrasound or fluoroscopy guidance for accurate, safe, and targeted injections
Injection into the correct anatomical plane or structure, whether it’s intra-articular, peritendinous, enthesis, or neural
Avoiding dilution or leakage into non-target tissues
Studies consistently show that image-guided PRP injections outperform blind injections, especially in deep or anatomically complex structures like the hip, sacroiliac joint, or cervical spine.
Age plays a pivotal role in response to biologic therapies like PRP. Older individuals often have:
Reduced baseline platelet function
Slower cellular response to growth factors
More advanced tissue degeneration
As a result, older patients typically require higher doses and more precisely tailored PRP formulations to achieve clinical benefit. This helps explain the higher variability in outcomes seen in the over-60 population, especially when treated with generic, low-concentration PRP.
Conversely, younger athletes with acute injuries and good healing potential may do well with lower doses and fewer injections — but again, only if delivered accurately and in the right setting.
PRP is not a one-size-fits-all therapy. Successful outcomes depend on:
Appropriate platelet dose and volume
Customisation for the condition and patient profile
Skillful, image-guided delivery
Clinical expertise in biologic medicine
So when we talk about PRP, we’re really talking about a spectrum of biologic tools that must be carefully selected and delivered. Understanding these nuances can help both patients and clinicians avoid disappointment — and better harness the healing potential of regenerative medicine.
📚 References
1. Fitzpatrick, J., Bulsara, M., Zheng, M. H. (2017). The effectiveness of platelet-rich plasma in the treatment of tendinopathy: A meta-analysis of randomized controlled clinical trials. The American Journal of Sports Medicine, 45(1), 226–233. https://doi.org/10.1177/0363546516643716
2. Andia, I., & Maffulli, N. (2018). Biological therapy for sports injuries. Biomolecules, 9(1), 1. https://doi.org/10.3390/biom9010001
3. Dhillon, M. S., Patel, S., & John, R. (2012). PRP in osteoarthritis knee – update, current confusions and future options. SICOT-J, 3, 24. https://doi.org/10.1051/sicotj/2016018
4. Mautner, K. R., et al. (2015). A call for standardization in platelet-rich plasma preparation. PM&R, 7(4), S43–S53. https://doi.org/10.1016/j.pmrj.2015.02.005
5. Anitua, E., et al. (2014). Influence of the preparation method on the characteristics of PRP. Clinical Orthopaedics and Related Research, 472, 3086–3093. https://doi.org/10.1007/s11999-014-3523-5
6. Dragoo, J. L., et al. (2014). Platelet-rich fibrin matrix autologous biologic treatment of patellar tendinopathy. The American Journal of Sports Medicine, 42(3), 610–618. https://doi.org/10.1177/0363546513518416
7. Dohan Ehrenfest, D. M., et al. (2014). Classification of platelet concentrates: From pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends in Biotechnology, 27(3), 158–167. https://doi.org/10.1016/j.tibtech.2008.11.009
8. Chahla, J., et al. (2017). Current concepts in the use of PRP for osteoarthritis of the knee. Sports Health, 9(3), 225–232. https://doi.org/10.1177/1941738117696846
9. Lana, J. F. S. D., et al. (2016). Leukocyte-rich PRP in the treatment of knee osteoarthritis. Current Reviews in Musculoskeletal Medicine, 9, 242–249. https://doi.org/10.1007/s12178-016-9344-2
10. Everts, P. A., et al. (2020). The role of PRP in regenerative medicine: Platelet biology, growth factors, and a practical approach. Journal of Functional Morphology and Kinesiology, 5(2), 34. https://doi.org/10.3390/jfmk5020034
11. Kon, E., et al. (2018). Platelet-rich plasma for the treatment of cartilage pathology. Current Reviews in Musculoskeletal Medicine, 11, 573–582. https://doi.org/10.1007/s12178-018-9521-7
12. Abbas, M., et al. (2022). Platelet-rich plasma dosage in osteoarthritis: A systematic review. Journal of Clinical Medicine, 11(11), 3067. https://doi.org/10.3390/jcm11113067
13. Patel, S., et al. (2013). Role of leukocyte-rich and leukocyte-poor PRP in knee osteoarthritis. The American Journal of Sports Medicine, 41(2), 356–364. https://doi.org/10.1177/0363546512471299
14. Piuzzi, N. S., et al. (2018). Platelet-rich plasma for the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. The Journal of Arthroplasty, 33(2), 280–297.e1. https://doi.org/10.1016/j.arth.2017.09.026
15. Moraes, V. Y., et al. (2014). Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database of Systematic Reviews, Issue 4. https://doi.org/10.1002/14651858.CD010071.pub3
16. Cervellin, M., et al. (2012). The effect of PRP concentrations on tenocytes: An in vitro study. International Orthopaedics, 36(5), 889–895. https://doi.org/10.1007/s00264-011-1351-4
17. Zaffagnini, S., et al. (2015). PRP vs hyaluronic acid in the treatment of knee OA. The American Journal of Sports Medicine, 43(7), 1575–1582. https://doi.org/10.1177/0363546515580787
18. Filardo, G., et al. (2015). Platelet-rich plasma in tendon-related disorders. Journal of Orthopaedic Surgery and Research, 10, 24. https://doi.org/10.1186/s13018-015-0163-3
19. Smith, P. A. (2016). Intra-articular PRP injections for knee osteoarthritis: Clinical outcomes and repeatability. The American Journal of Sports Medicine, 44(4), 884–891. https://doi.org/10.1177/0363546515609591
20. Andia, I., & Maffulli, N. (2021). New insights into PRP therapeutics: Refined classification and dose-response relationships. Expert Opinion on Biological Therapy, 21(6), 759–774. https://doi.org/10.1080/14712598.2021.1903364