Email : admin@mskdoc.co.nz | Phone : 02727 00100
Opening Hours : Mon-Friday : 10 AM – 4 PM
Email : admin@mskdoc.co.nz | Phone : 02727 00100
Opening Hours : Mon-Friday : 10 AM – 4 PM
Email : admin@mskdoc.co.nz | Phone : 02727 00100 | Opening Hours : Mon-Friday : 10 AM – 4 PM
By: Dr Zaid Matti
Musculoskeletal Medicine Specialist
Plantar fasciitis is one of the most common causes of chronic heel pain, affecting up to 10% of the population at some point. It involves microtears and degeneration of the plantar fascia—often resistant to conventional treatments in long-standing cases

🧪 PRP Therapy: Healing with Your Own Blood
Platelet-Rich Plasma (PRP) involves concentrating a patient’s own platelets and injecting them into the diseased fascia. These platelets release growth factors (e.g., PDGF, TGF-β, VEGF) that can:
📊 What Does the Latest Research Say?
The evidence for PRP in chronic plantar fasciitis is increasingly robust.
🔍 Newly Added Key Studies:
📚 Other Supporting Evidence
🌱 Benefits of PRP for Heel Pain
⚠️ Clinical Considerations
🧠 Bottom Line
PRP is a safe, evidence-backed option for treating chronic plantar fasciitis, with data consistently supporting its superiority over corticosteroids for long-term outcomes. For patients looking to avoid surgery or repeated steroid injections, it offers a regenerative, biologically intelligent alternative.
🔬 References
The procedure is typically done in an outpatient clinic and involves:
Blood Collection: A small amount of your blood is drawn from your arm.
Platelet Concentration: The blood is processed in a centrifuge to isolate and concentrate platelets.
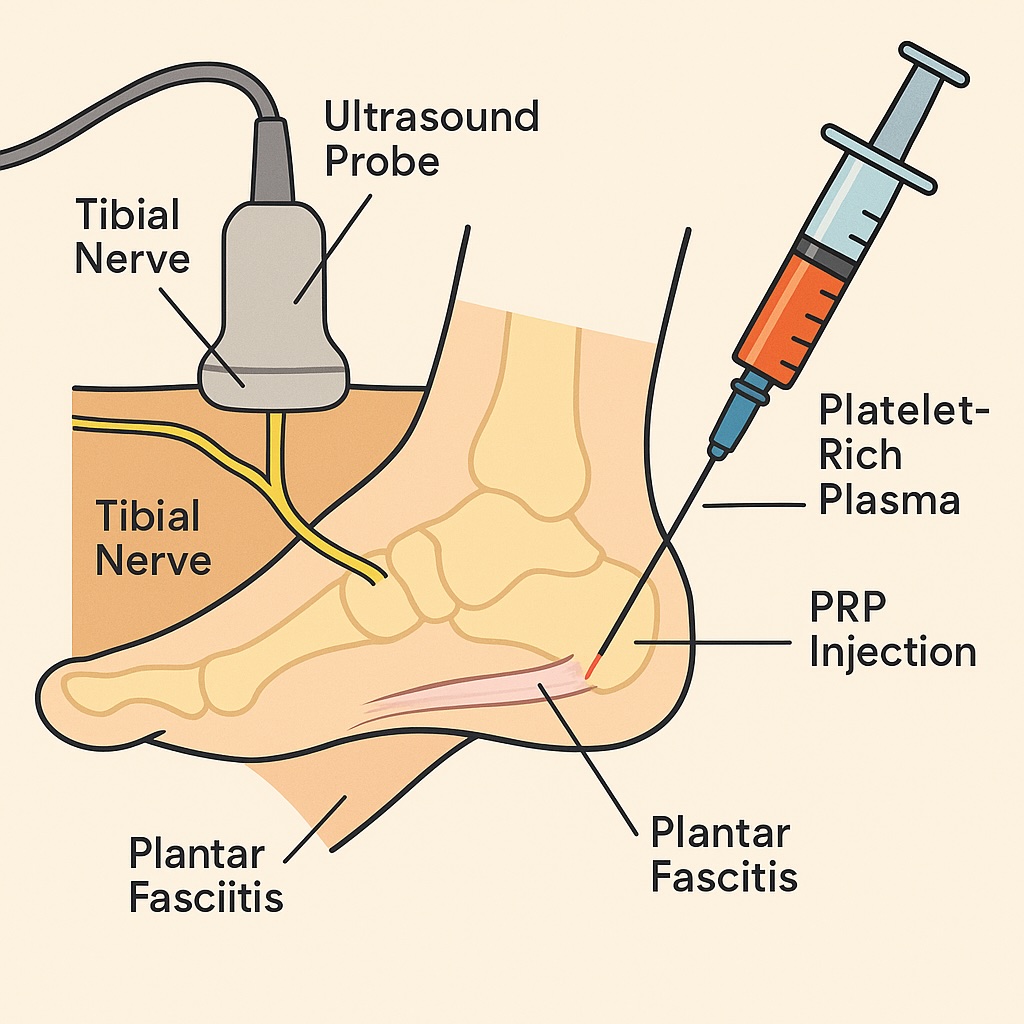
Ultrasound-Guided Injection: Using high-resolution ultrasound, the physician identifies the precise area of degeneration in the plantar fascia.
Tibial Nerve Block: A local tibial nerve block is often used to numb the foot, making the procedure more comfortable.
Precise PRP Injection: The concentrated PRP is then injected into the plantar fascia or its enthesis (where the tissue attaches to bone), under ultrasound guidance to ensure accuracy.
This targeted technique helps deliver the healing factors exactly where they are needed, while minimising discomfort during and after the procedure.